New Jersey Health Information Exchange Operational Plan: August 13, 2010
Includes Map of Current HIE Landscape
New Jersey sent its Operational Plan for State Health Information Exchange Cooperation Agreement to the Office of the National Coordinator for Health IT on August 13, 2010. Per the report, New Jersey submitted its initial “State HIT Plan in October 2009 with an additional update in January 2010.” Plan is posted on NJ Health IT Commission Web site, with excerpts below which include the cover letter from NJ State HIE Coordinator Colleen Woods and the Executive Summary.
[Clicking on any of the four figures will give you a clearer view of those figures.]
Operational Plan PDF [2.2M]
COVER LETTER
August 13, 2010
David Blumenthal MD, MPP
National Coordinator for Health Information Technology
Department of Health and Human Services
Washington, DC 20201
Dear Dr. Blumenthal:
Attached is New Jersey’s HIT Operational Plan which represents a continuation of our planning efforts started in 2009 with the submission to the Office of the National Coordinator for HIT of our State HIT Plan in October 2009 with an additional update in January 2010. Our Operational Plan represents a significant collaborative effort that included:
- New Jersey State Medicaid leadership
- Director of NJ-HITEC, our Regional Extension Center
- Executive Director of the New Jersey HIT Commission
- Director of the New Jersey Office for eHIT Development
- Leadership from our four funded HIEs
- Leaders from several unfunded HIEs
- Representative from New Jersey Hospital Association
I am very pleased with the result and believe this represents a significant step for the State of New Jersey in bringing fundamental change in the delivery, quality, and value of healthcare in the State. With this Plan we bring:
- A re- commitment for New Jersey to be a national leader in HIT
- A drive to leverage and harness health information to improve, monitor and protect the health of our citizens
- A goal to meet and exceed Federal mandates for each person to have an electronic health record by 2014
As the New Jersey Statewide HIT Coordinator I am committed to working with all state departments and agencies, the healthcare provider community, and other key stakeholders, to implement and facilitate the HIT Strategic and Operational Plans for New Jersey in accordance with nationally recognized Federal standards.We look forward to your timely review and approval of our HIT Operational Plan and continued collaboration on this vital issue for our country and for the State of New Jersey. We also request timely release of implementation funds for our four ONC funded HIEs.
Sincerely,
Ms. Colleen Woods
New Jersey Statewide HIT Coordinator
NEW JERSEY STATE OPERATIONAL PLAN
Submitted August 13, 2010
1.0 EXECUTIVE SUMMARY
This HIT Operational Plan serves as the approach and schedule to implement New Jersey’s Strategic HIT Plan previously submitted in October 2009 and further refined in January 2010. Execution of this Plan will enhance the quality, delivery, and value of healthcare while supporting New Jersey’s hospitals and eligible providers in achieving and demonstrating meaningful use of Health Information Technology (HIT). The State acknowledges that the HIT and HIE landscape at the federal and state levels is evolving, and that this is a living document requiring ongoing review, changes, and refinement. Our plan, by design, is nimble and adaptable to the expected changes and evolution of HIT strategy.
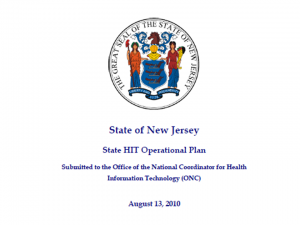
A Unique Approach - Our approach, depicted in Figure 1.1 below, builds on existing, long-standing HIT projects across the State combined with newly funded ARRA initiatives to ensure that all expenditures and resources are leveraged in one cohesive, strategic plan. Recognizing that complex and functional HIT systems are already established, and that expertise is available and willing to be shared, building our plan on a “ground-up” strategy makes perfect sense. Realizing that barriers do exist, our leadership is committed to identifying and eliminating barriers, while ensuring that duplication of effort and expenses are avoided. 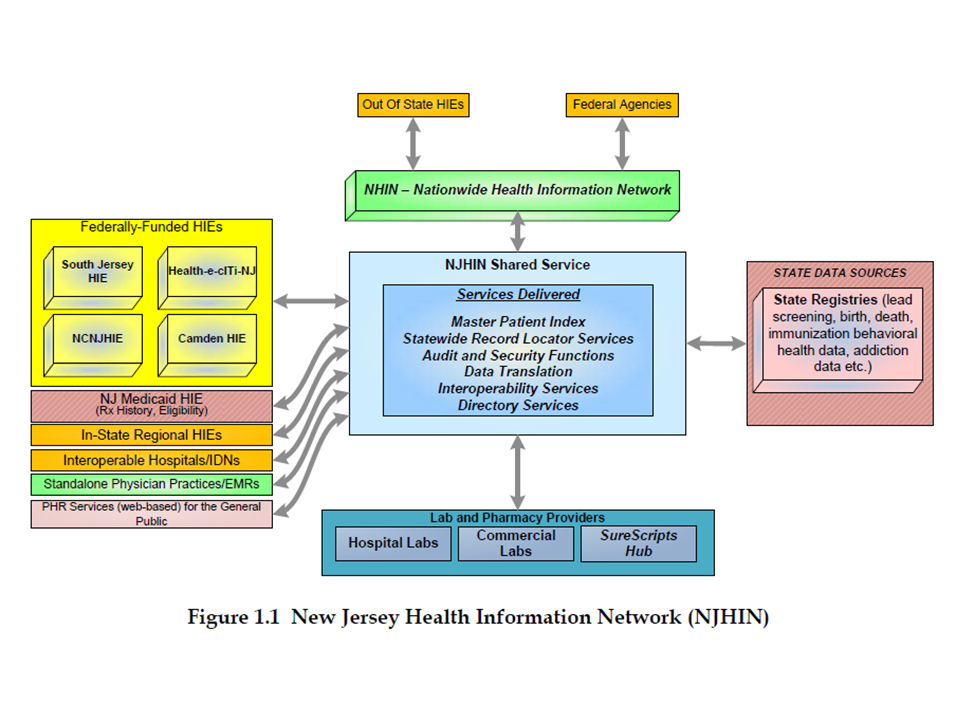
Figure 1.1 New Jersey Health Information Network (NJHIN)
Our approach recognizes that this is a time of unprecedented change in the Heath Information Technology landscape. Simultaneously, the following conditions and projects are occurring across New Jersey:
- Community-based physicians are moving to better understand the impact of adopting certified electronic health record (EHR) technology in order to be eligible for “meaningful use” incentives.
- Hospitals are expanding and upgrading their IT systems to ensure “meaningful use” eligibility as well.
- The newly created regional extension center, the New Jersey Health Information Technology Extension Center (NJ-HITEC) has begun to assist physicians in understanding EHR technology, selecting technology vendors and becoming eligible for “meaningful use” incentives.
- Four ONC funded regional Health Information Exchanges (HIEs) are in various stages of becoming incorporated, developing solution strategies and building/testing new infrastructure. Health-e-cITi-NJ has been incorporated as a 501(c)(3) organization. Jersey Health Connect has been incorporated and is awaiting 501(c)(3) designation.
- No less than eight distinct HIE models have been identified throughout the State that are in a position to be leveraged into the state plan.
- New Jersey Medicaid is progressing toward its own HIE model and has begun implementation of a crucial Master Client Index project.
The New Jersey Health Information Network (NJHIN) will integrate these various projects and initiatives. In effect, NJHIN consists of a “network of networks” in which centralized shared services will provide:
- A focal point for accessing state-managed data (e.g., various state registries).
- A record locator service (RLS) for locating records within the four new regional HIEs, the Medicaid HIE and the other existing HIE initiatives across the State.
- A conduit to the federal NHIN Direct and NHIN Connect networks.
Key aspects of the NJHIN include:
- Leveraging of significant work in progress through a “ground up” collaborative effort between state HIT leadership and several community-based healthcare organizations within the State.
- A multi-track effort leveraging Medicaid capabilities and funding, local HIE leadership, provider capabilities, NJ-HITEC services, and overall state HIT leadership.
- A centralized approach where appropriate, e.g., Master Patient Index/Master Client Index, while leveraging community based innovation and leadership.
- NJHIN will leverage Medicaid and all the MMIS medical history data that already exists for ~1.3M citizens in our state representing 15% of our population.
Significant effort and investment have already been made in evolving the NJHIN. The release of implementation funding for the four approved HIEs will accelerate the realization of the NJHIN.
Continuing Our Leadership – New Jersey has been in the forefront of promoting electronic health records. Some historical context includes:
- New Jersey’s active interest in electronic systems as a means of increasing healthcare quality and reducing costs began in 1993 through a study to analyze current methods, barriers, and recommendations for achieving savings and administrative simplification in the New Jersey healthcare system.
- This led to the passage of the New Jersey Health Information Network and Technology (HINT) law in 1999 which set a precedent for health information technology standards for interoperability in the Garden State.
- During 2004-2005 the New Jersey Hospital Association began facilitating discussion focused on HIE development and deployment. This led to the emergence of several community-based HIE initiatives which have become the basis of the current NJHIN.
- As early as 2004, some New Jersey hospital systems began developing HIE models, primarily within their corporate structures, and have accomplished sophisticated health information sharing solutions that are ready to be integrated into the statewide plan.
- In 2008 the New Jersey Health Information Technology Act was passed which mandates the creation of a plan to implement a secure, integrated, inter-operative and statewide infrastructure for the sharing of electronic health records. The Act also created a Health Information Technology Commission to oversee the development, implementation and oversight of the plan, in partnership with the Office for eHIT Development.
- In October 2009 New Jersey submitted one of the first State HIT Plans to ONC and received initial approval of the four requested HIE implementation grants.
- In March 2010, through a transformation grant from CMS, the New Jersey Division of Medical Assistance and Health Services (DMAHS) initiated a project to build Phase I of our Master Patient Identifier (MPI) capability which will promote the critical interoperable exchange of Medicaid, Immunization, and Blood Lead Screening databases among New Jersey’s departments of Health and Senior Services and Children and Families, Managed Care Organizations, Federally Qualified Health Center (FQHC) providers, hospitals and the Department of Human Services.
• In March of 2010, DMHAS initiated a Planning APD to CMS to secure planning funds to begin the State Medicaid HIT Plan (SMHP) that will be leveraged and integrated into the statewide planning process.
• Implementation planning is underway for the NJ-HITEC which will promote broad-based adoption of electronic health records. Funding for this effort was received in mid-2010.
Our leadership continues at the national and state level as we aggressively move forward in transforming the healthcare delivery system of New Jersey.
Our Fundamental Strategies – In addition to supporting the strategic direction articulated in our State HIT Plan submitted in October 2009, the following represents the fundamental strategies for our HIT Operational Plan. These strategies include the following:
- Medicaid is a key partner in the execution of this HIT Operational Plan and we will leverage CMS funding to help build the infrastructure for statewide health information exchange.
- A core tenet of the program is the elimination of disparities of care by ensuring that underserved communities, including children, are represented in evolving HIT/HIE efforts. We must also be aware of the potential for a “digital divide” between more affluent segments of the population and those who are underserved.
- We will leverage our 98% broadband coverage (#1 in the US) to ensure all providers and healthcare service recipients have access to the right information at the right time.
- We will leverage all funding sources (public and private) to ensure the financial viability and stability of the HIT program.
- Through effective HIT coordination we will eliminate duplicative efforts and projects across the HIT landscape and ensure efficiency of efforts by centralizing and sharing policies, standards, and infrastructure as appropriate.
- We will effectively manage the transformational change in the New Jersey healthcare community through the efforts of the NJ-HITEC and the Office of the Statewide HIT Coordinator.
Coordinating Our Efforts – Ms. Colleen Woods has recently been named as New Jersey’s Statewide HIT Coordinator. Among her many outstanding qualifications Ms. Woods was most recently the CIO for the New Jersey Department of Human Services providing technology direction to the State Medicaid Program. With her selection, we have adjusted our overall governance structure for the HIT Program pertaining to HIT direction and policy. As depicted below the Program is wide-ranging with a varied and complex set of stakeholders.
Figure 1.2 New Jersey HIT Program Context
Effective governance is essential. Given this context we have designed and implemented a governance capability to drive successful program performance and results.
 Figure 1.3 New Jersey HIT Program Governance
Figure 1.3 New Jersey HIT Program Governance
The ongoing transformation of the healthcare system in New Jersey from a paper-based healthcare information environment to a digital healthcare information environment is complex and will require collaboration between multiple parties with potential conflicting interests. We are confident our approach will build upon our early successes in bringing together the necessary constituents (both public and private) to continue the transformation to provide access to reliable healthcare information that improves the quality and efficiency of care.
***************************************************
As described in this Operational Plan, the State acknowledges and accepts the following HIT program responsibilities:
- To ensure alignment with Medicaid and other public health programs.
- To design and manage a transparent multi-stakeholder process to guide and implement the program.
- To monitor and track meaningful use of HIE capabilities through a well-coordinated and effective communication process.
- To ensure the accuracy, security, and privacy of personal health records.
- To assure all stakeholders that information sharing is consistent with state and federal security and privacy provisions.
- To ensure effective gap closing strategies related to HIE capabilities for meaningful use exist and are effectively managed.
- To educate the public (patients and providers alike) to understand, embrace, and realize the benefits of EHR technology.
- To take the lead in developing statewide, standardized policies and procedures that are consistent with those established at the national level.
In addition to the technical aspects of establishing the NJHIN, the HIT Operational Plan addresses the regulatory, financial sustainability, governance, and project management approaches to effectively implement our strategies. The sections that follow begin with the HIT Operational Plan requirements (highlighted) from the State Health Information Exchange Cooperative Agreement Program Funding Opportunity Announcement (FOA) and the related Program Information Notice (PIN), dated July 6, 2010, followed by our response.
This HIT Operational Plan is submitted to the Office of the National Coordinator for Health Information Technology (ONC) for review and approval.
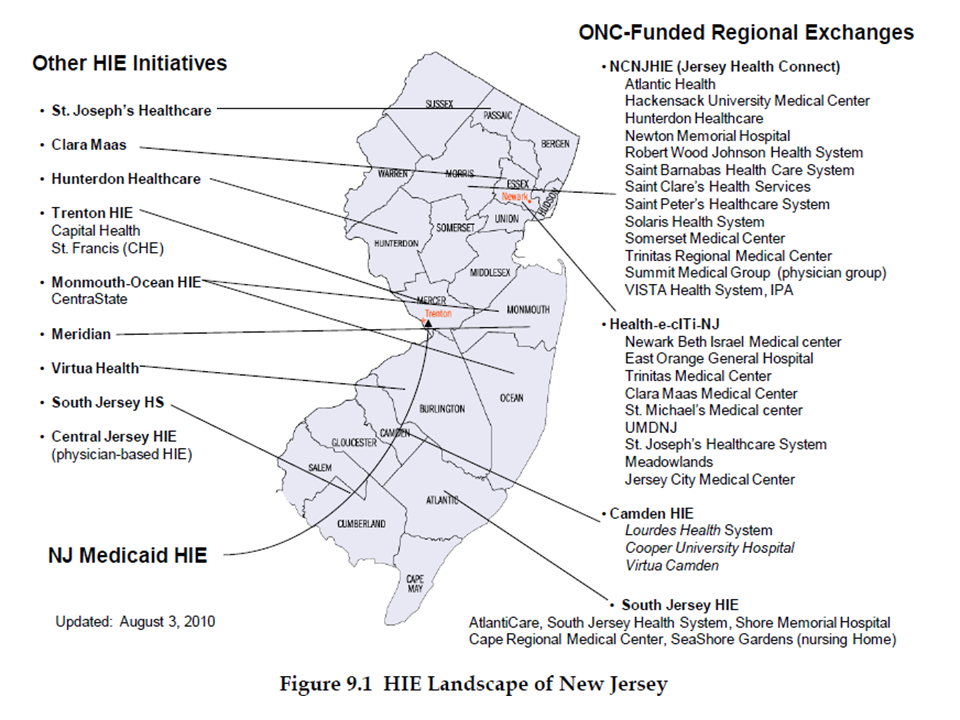
HIE Landscape in New Jersey
Excerpted from Section 9.0 HIE ARCHITECTURE AND STANDARDS
[Clicking on the map below will give you a clearer view of the map.]
# # #

