SECRETARY SEBELIUS ANNOUNCES FINAL RULES TO SUPPORT MEANINGFUL USE OF ELECTRONIC HEALTH RECORDS
July 13, 2010 Press Release from Centers for Medicare and Medicaid Services
Plus PDFs of Final Rules, Joint ONC/CMS Fact Sheet,
ONC and CMS Fact Sheets and FAQs
Blumenthal article from NEJM with Summary Matrix
————————————————————————————————
KEY LINKS:
Summary of
The “Meaningful Use” Regulation for Electronic Health Records
By David Blumenthal, MD, MPP, National Coordinator for Health IT
and Marilyn Tavenner, RN, MHA, Principal Deputy Administrator of CMS
New England Journal of Medicine, July 13, 2010
Includes matrix with Summary Overview of Meaningful Use Objectives
HTML Version PDF Version
Finding My Way to Electronic Health Records
By Regina Benjamin, MD, MBA, Surgeonn General, US Public Health Service
New England Journal of Medicine, July 13, 2010
HTML Version PDF Version
FINAL RULES
Medicare and Medicaid Programs;
Electronic Health Record Incentive Program [PDF]
http://www.ofr.gov/OFRUpload/OFRData/2010-17207_PI.pdf
Health Information Technology:
Initial Set of Standards, Implementation Specifications,
and Certification Criteria
for Electronic Health Record Technology [PDF]
http://www.ofr.gov/OFRUpload/OFRData/2010-17210_PI.pdf
———————————————————————————————
July 13, 2010 Press Release from CMS:
WASHINGTON – U.S. Department of Health and Human Services Secretary Kathleen Sebelius today announced final rules to help improve Americans’ health, increase safety and reduce health care costs through expanded use of electronic health records (EHR).

HHS Secretary Kathleen Sebelius
“For years, health policy leaders on both sides of the aisle have urged adoption of electronic health records throughout our health care system to improve quality of care and ultimately lower costs,” Secretary Sebelius said. “Today, with the leadership of the President and the Congress, we are making that goal a reality.”
Under the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, eligible health care professionals and hospitals can qualify for Medicare and Medicaid incentive payments when they adopt certified EHR technology and use it to achieve specified objectives. One of the two regulations announced today defines the “meaningful use” objectives that providers must meet to qualify for the bonus payments, and the other regulation identifies the technical capabilities required for certified EHR technology.
Announcement of today’s regulations marks the completion of multiple steps laying the groundwork for the incentive payments program. With “meaningful use” definitions in place, EHR system vendors can ensure that their systems deliver the required capabilities, providers can be assured that the system they acquire will support achievement of “meaningful use” objectives, and a concentrated five-year national initiative to adopt and use electronic records in health care can begin.
“This is a turning point for electronic health records in America , and for improved quality and effectiveness in health care,” said David Blumenthal, M.D., National Coordinator for Health Information Technology. “In delivering on the goals that Congress called for, we have sought to provide the leadership and coordination that are essential for a large, technology-based enterprise. At the same time, we have sought and received extensive input from the health care community, and we have drawn on their experience and wisdom to produce objectives that are both ambitious and achievable.”
Two companion final rules were announced today. One regulation, issued by the Centers for Medicare & Medicaid Services (CMS), defines the minimum requirements that providers must meet through their use of certified EHR technology in order to qualify for the payments. The other rule, issued by the Office of the National Coordinator for Health Information Technology (ONC), identifies the standards and certification criteria for the certification of EHR technology, so eligible professionals and hospitals may be assured that the systems they adopt are capable of performing the required functions.
As much as $27 billion may be expended in incentive payments over ten years. Eligible professionals may receive as much as $44,000 under Medicare and $63,750 under Medicaid, and hospitals may receive millions of dollars for implementation and meaningful use of certified EHRs under both Medicare and Medicaid.
The CMS rule announced today makes final a proposed rule issued on Jan, 13, 2010. The final rule includes modifications that address stakeholder concerns while retaining the intent and structure of the incentive programs. In particular, while the proposed rule called on eligible professionals to meet 25 requirements (23 for hospitals) in their use of EHRs, the final rules divides the requirements into a “core” group of requirements that must be met, plus an additional “menu” of procedures from which providers may choose. This “two track” approach ensures that the most basic elements of meaningful EHR use will be met by all providers qualifying for incentive payments, while at the same time allowing latitude in other areas to reflect providers’ needs and their individual path to full EHR use.
“CMS received more than 2,000 comments on our proposed rule,” said Marilyn Tavenner, Principal Deputy Administrator of CMS. “Many comments were from those who will be most immediately affected by EHR technology – health care providers and patients. We carefully considered every comment and the final meaningful use rules incorporate changes that are designed to make the requirements achievable while meeting the goals of the HITECH Act.”
Requirements for meaningful use incentive payments will be implemented over a multi-year period, phasing in additional requirements that will raise the bar for performance on IT and quality objectives in later years. The final CMS rule specifies initial criteria that eligible professionals (EPs) and eligible hospitals, including critical access hospitals (CAHs), must meet. The rule also includes the formula for the calculation of the incentive payment amounts; a schedule for payment adjustments under Medicare for covered professional services and inpatient hospital services provided by EPs, eligible hospitals and CAHs that fail to demonstrate meaningful use of certified EHR technology by 2015; and other program participation requirements.
Key changes in the final CMS rule include:
- Greater flexibility with respect to eligible professionals and hospitals in meeting and reporting certain objectives for demonstrating meaningful use. The final rule divides the objectives into a “core” group of required objectives and a “menu set” of procedures from which providers may choose any five to defer in 2011-2012. This gives providers latitude to pick their own path toward full EHR implementation and meaningful use.
- An objective of providing condition-specific patient education resources for both EPs and eligible hospitals and the objective of recording advance directives for eligible hospitals, in line with recommendations from the Health Information Technology Policy Committee.
- A definition of a hospital-based EP as one who performs substantially all of his or her services in an inpatient hospital setting or emergency room only, which conforms to the Continuing Extension Act of 2010
- CAHs within the definition of acute care hospital for the purpose of incentive program eligibility under Medicaid.
CMS’ and ONC’s final rules complement two other recently issued HHS rules. On June 24, 2010, ONC published a final rule establishing a temporary certification program for health information technology. And on July 8, 2010 the Office for Civil Rights announced a proposed rule that would strengthen and expand privacy, security, and enforcement protections under the Health Insurance Portability and Accountability Act of 1996.
As part of this process, HHS is establishing a nationwide network of Regional Extension Centers to assist providers in adopting and using in a meaningful way certified EHR technology.
“Health care is finally making the technology advances that other sectors of our economy began to undertake years ago,” Dr. Blumenthal said. “These changes will be challenging for clinicians and hospitals, but the time has come to act. Adoption and meaningful use of EHRs will help providers deliver better and more effective care, and the benefits for patients and providers alike will grow rapidly over time.”
A CMS/ONC fact sheet on the rules is available at http://www.cms.gov/EHRIncentivePrograms/
Technical fact sheets on CMS’s final rule are available at http://www.cms.gov/EHRIncentivePrograms/
A technical fact sheet on ONC’s standards and certification criteria final rule is available at http://healthit.hhs.gov/standardsandcertification.
RULES:
Medicare and Medicaid Programs; Electronic Health Record Incentive Program [PDF]
http://www.ofr.gov/OFRUpload/OFRData/2010-17207_PI.pdf
Health Information Technology: Initial Set of Standards, Implementation Specifications, and Certification Criteria for Electronic Health Record Technology [PDF]http://www.ofr.gov/OFRUpload/OFRData/2010-17210_PI.pdf
# # # # # # #
ONC: Electronic Health Records and Meaningful Use
Information for Providers
Information for Consumers
Information excerpted from ONC pages on July 13, 2010.
Electronic health records can provide many benefits for providers and their patients:
- Complete and accurate information. With electronic health records, providers have the information they need to provide the best possible care.Providers will know more about their patients and their health history before they walk into the examination room.
- Better access to information. Electronic health records facilitate greater access to the information providers need to diagnose health problems earlier and improve the health outcomes of their patients. Electronic health records also allow information to be shared more easily among doctors’ offices, hospitals, and across health systems, leading to better coordination of care.
- Patient empowerment. Electronic health records will help empower patients to take a more active role in their health and in the health of their families. Patients can receive electronic copies of their medical records and share their health information securely over the Internet with their families.
Currently, most health care providers still use medical record systems based on paper. New government incentives and programs are helping health care providers across the country make the switch to electronic health records.
Why Electronic Health Records?
Electronic health records can improve care by enabling functions that paper medical records cannot deliver:
- EHRs can make a patient’s health information available when and where it is needed – too often care has to wait because the chart is in one place and needed in another. EHRs enable clinicians secure access to information needed to support high quality and efficient care
- EHRs can bring a patient’s total health information together to support better health care decisions, and more coordinated care
- EHRs can support better follow-up information for patients – for example, after a clinical visit or hospital stay, instructions and information for the patient can be effortlessly provided; and reminders for other follow-up care can be sent easily or even automatically to the patient.
- EHRs can improve patient and provider convenience – patients can have their prescriptions ordered and ready even before they leave the provider’s office, and insurance claims can be filed immediately from the provider’s office.
Background: Legislation and RegulationsThe Health Information Technology for Economic and Clinical Health (HITECH) Act provides HHS with the authority to establish programs to improve health care quality, safety, and efficiency through the promotion of health information technology (HIT), including electronic health records and private and secure electronic health information exchange.Under HITECH, eligible health care professionals and hospitals can qualify for Medicare and Medicaid incentive payments when they adopt certified EHR technology and use it to achieve specified objectives. Two regulations have been released, one of which defines the “meaningful use” objectives that providers must meet to qualify for the bonus payments, and the other which identifies the technical capabilities required for certified EHR technology.
- Incentive Program for Electronic Health Records: Issued by the Centers for Medicare & Medicaid Services (CMS), this final rule defines the minimum requirements that providers must meet through their use of certified EHR technology in order to qualify for the payments.
- Standards and Certification Criteria for Electronic Health Records: Issued by the Office of the National Coordinator for Health Information Technology, this rule identifies the standards and certification criteria for the certification of EHR technology, so eligible professionals and hospitals may be assured that the systems they adopt are capable of performing the required functions.
JOINT ONC/CMS FACT SHEET
CMS AND ONC FINAL REGULATIONS DEFINE MEANINGFUL USE AND SET STANDARDS FOR ELECTRONIC HEALTH RECORD INCENTIVE PROGRAM
Excerpted from CMS site on July 13, 2010.
The Centers for Medicare & Medicaid Services (CMS) and the Office of the National Coordinator for Health Information Technology (ONC) today announced two complementary final rules to implement the electronic health records (EHR) incentive program under the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Enacted as part of the American Recovery and Reinvestment Act (ARRA) of 2009, the HITECH Act supports the adoption of electronic health records by providing financial incentives under Medicare and Medicaid to hospitals and eligible professionals who implement and demonstrate “meaningful use” certified EHR technology. The CMS regulations announced today specify the objectives that providers must achieve in payment years 2011 and 2012 to qualify for incentive payments; the ONC regulations specify the technical capabilities that EHR technology must have to be certified and to support providers in achieving the “meaningful use” objectives.
The final CMS rule:
- Specifies initial criteria that eligible professionals (EPs), eligible hospitals, and critical access hospitals (CAHs) must meet to demonstrate meaningful use and qualify for incentive payments.
- Includes both “core” criteria that all providers must meet to qualify for payments, while also allowing provider choice among a “menu set” of additional criteria.
- Outlines a phased approach to implement the requirements for demonstrating meaningful use. This approach initially establishes criteria for meaningful use based on currently available technological capabilities and providers’ practice experience. CMS will establish graduated criteria for demonstrating meaningful use through future rulemaking, consistent with anticipated developments in technology and providers’ capabilities.
The CMS rule finalizes a Notice of Proposed Rulemaking published on Jan 13, 2010.
The final ONC rule:
- Sets initial standards, implementation specifications, and certification criteria for EHR technology under the incentive program.
- Coordinates the standards required of EHR systems with the meaningful use requirements for eligible professionals and hospitals
- With these standards in place, providers can be assured that the certified EHR technology they adopt is capable of performing the required functions to comply with CMS’ meaningful use requirements and other administrative requirements of the Medicare and Medicaid EHR incentive programs.
ONC’s standards and certification criteria final rule completes the adoption of an initial set of standards, implementation specifications and certification criteria that was begun with publication of ONC’s on Jan. 13, 2010.
Timetable for Implementation
The HITECH Act states that payments for Medicare providers may begin no sooner than October 2010 for eligible hospitals and January 2011 for EPs. The final rule aligns the Medicare and Medicaid program start dates. Key steps in the implementation timeline include:
ONC began accepting applications from entities that seek approval as an ONC-Authorized Testing and Certification Body (ONC-ATCB) on July 1, 2010.
ONC projects that certified EHR software will be available for purchase by hospitals and eligible professionals by fall, 2010.
- Registration by both EPs and eligible hospitals with CMS for the EHR incentive program will begin in January 2011. Registration for both the Medicare and Medicaid incentive programs will occur at one virtual location, managed by CMS.
- For the Medicare program, attestations may be made starting in April 2011 for both EPs and eligible hospitals.
- Medicare EHR incentive payments will begin in mid May 2011.
- States will be initiating their incentive programs on a rolling basis, subject to CMS approval of the State Medicaid HIT plan, which details how each State will implement and oversee its incentive program.
The “Meaningful Use” Model
By focusing on the effective use of EHRs with certain capabilities, the HITECH Act makes clear that the adoption of records is not a goal in itself: it is the use of EHRs to achieve health and efficiency goals that matters. HITECH’s incentives and assistance programs seek to improve the health of Americans and the performance of their health care system through “meaningful use” of EHRs to achieve five health care goals:
- To improve the quality, safety, and efficiency of care while reducing disparities;
- To engage patients and families in their care;
- To promote public and population health;
- To improve care coordination; and
- To promote the privacy and security of EHRs.
In the context of the EHR incentive programs, “demonstrating meaningful use” is the key to receiving the incentive payments. It means meeting a series of objectives that make use of EHRs’ potential and related to the improvement of quality, efficiency and patient safety in the healthcare system through the use of certified EHR technology.
Coordinated Approach to Support EHR Adoption
CMS’ and ONC’s final rules complement two other rules that were recently issued. On June 24, 2010, ONC published a final rule to establish a temporary certification program for health information technology. And on July 8, 2010, the Office for Civil Rights announced a proposed rule that would strengthen and expand privacy, security, and enforcement protections under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
Together the four rules are key components of the regulatory structure needed to administer the EHR incentive program and to meet the goals of the HITECH Act:
The assurance of privacy protections is fundamental to the success of EHR adoption. The refinements and expansions of HIPAA provisions announced July 8 form an important base for EHR acceptance and use.
- The temporary certification process published June 24 establishes a process through which organizations can be approved as certifying entities to which vendors may submit their EHR systems for review and certification.
- The ONC rule announced today identifies the technical standards which must be met in the certification process, and coordinates those requirements with the meaningful use objectives.
- Finally, the CMS rule announced today establishes guidelines and requirements on achieving meaningful use in clinical settings and qualifying for incentive payments based on this meaningful use.
Key Provisions of the Final Rule
CMS’s final meaningful use rule incorporates changes from the proposed rule on meaningful use that are designed to make the requirements more readily achievable while meeting the goals of the HITECH Act. For Stage 1, which begins in 2011, the criteria for meaningful use focus on electronically capturing health information in a coded format, using that information to track key clinical conditions, communicating that information for care coordination purposes, and initiating the reporting of clinical quality measures and public health information.
The final rule reflects significant changes to the proposed rule while retaining the intent and structure of the incentive programs. Key provisions in the final rule include:
- For Stage 1, CMS’s proposed rule called on physicians and other eligible professionals to meet 25 objectives (23 for hospitals) in reporting their meaningful use of EHRs. The final rule divides the objectives into a “core” group of required objectives and a “menu set” of procedures from which providers can choose. This “two track” approach ensures that the most basic elements of meaningful EHR use will be met by all providers qualifying for incentive payments, while at the same time allowing latitude in other areas to reflect providers’ varying needs and their individual paths to full EHR use.
- In line with recommendations of the Health Information Technology Policy Committee, the final rule includes the objective of providing patient-specific educational resources for both EPs and eligible hospitals and the objective of recording advance directives for eligible hospitals.
- With respect to defining hospital-based physicians, the final rule conforms to the Continuing Extension Act of 2010. That law addressed provider concerns about hospital-based providers in ambulatory settings being unable to qualify for incentive payments by defining a hospital-based EP as performing substantially all of his or her services in an inpatient hospital setting or emergency room only.
- The rule makes final a proposed rule definition that would make individual payments to eligible hospitals identified by their individual CMS Certification Number. The final rule retains the proposed definition of an eligible hospital because that is most consistent with policy precedents in how Medicare has historically applied the statutory definition of a ”subsection (d)” hospital under other hospital payment regulations.
- Under Medicaid, the final rule includes critical access hospitals (CAHs) in the definition of acute care hospital for the purpose of incentive program eligibility.
The final rule’s economic analysis estimates that incentive payments under Medicare and Medicaid EHR programs for 2011 through 2019 will range from $9.7 billion to $27.4 billion.
Development of the Rules
CMS and ONC worked closely to develop the two rules and received input from hundreds of technical subject matters experts, health care providers, consumers, and other key stakeholders. Numerous public meetings to solicit public comment were held by three Federal advisory committees: the National Committee on Vital and Health Statistics (NCVHS), the HIT Policy Committee (HITPC), and the HIT Standards Committee (HITSC). HITSC presented its final recommendations to the National Coordinator in August 2009.
CMS published its proposed rule on Jan. 13, 2010. The agency actively solicited comments on its proposal and received more than 2,000 submissions by the close of the 60-day comment period. These comments, along with the input from advisory groups and outreach activities, were given careful consideration in developing the regulations announced today.
# # #
ELECTRONIC HEALTH RECORDS AT A GLANCE
CMS FACT SHEET With Frequently Asked Questions
Excerpted from CMS site on July 14, 2010.
“Our recovery plan will invest in electronic health records and new technology that will reduce errors, bring down costs, ensure privacy and save lives.”
- President Obama, Address to Joint Session of Congress, February 2009
Background
As promised by the President, the American Recovery and Reinvestment Act of 2009 included under which, according to current estimates, as much as $27 billion over ten years will be expended to support adoption of electronic health records (EHRs). While there has been bipartisan support for EHR adoption for at least half a decade, this is the first substantial commitment of federal resources to support adoption and help providers identify the key functions that will support improved care delivery.
Under the Health Information Technology for Economic and Clinical Health Act (HITECH), federal incentive payments will be available to doctors and hospitals when they adopt EHRs and demonstrate use in ways that can improve quality, safety and effectiveness of care. Eligible professionals can receive as much as $44,000 over a five-year period through Medicare. For Medicaid, eligible professionals can receive as much as $63,750 over six years. Medicaid providers can receive their first year’s incentive payment for adopting, implementing and upgrading certified EHR technology but must demonstrate meaningful use in subsequent years in order to qualify for additional payments.
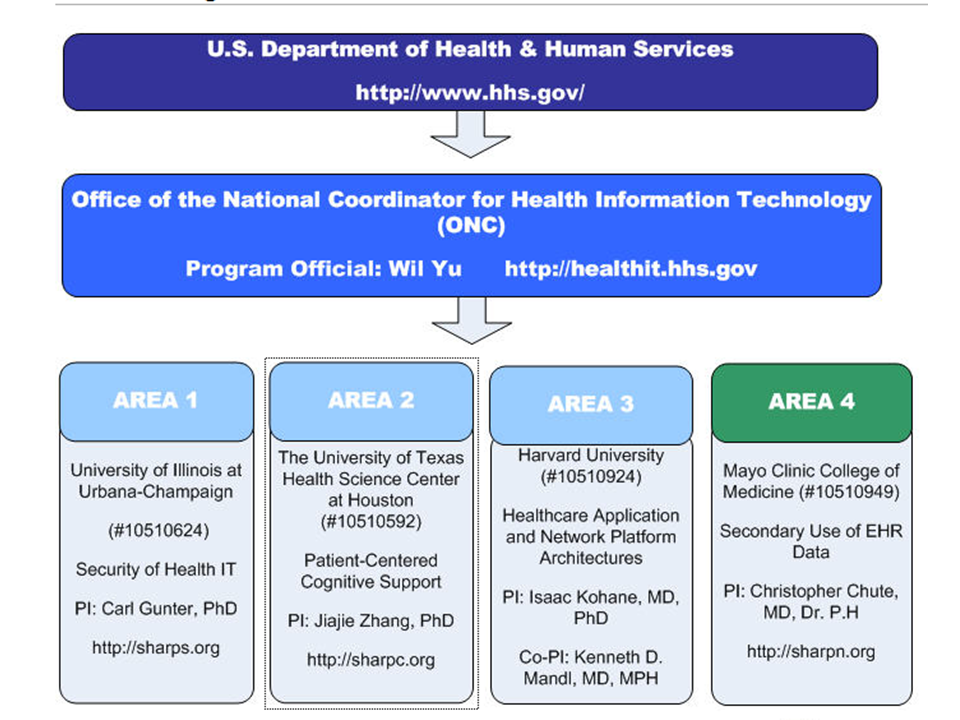
Since enactment of HITECH in February 2009, the Office of the National Coordinator for Health Information Technology (ONC), the Centers for Medicare & Medicaid Services (CMS) and other HHS agencies have been laying the groundwork for the massive national investment in EHRs:
- Creation of Regional Extension Centers (RECs) to support providers in adopting EHRs
- Developing workforce training programs
- Identifying “Beacon Communities” that lead the way in adoption and use of EHRs
- Developing capabilities for information exchange, including building toward a Nationwide Health Information Network
- Improving privacy and security provisions of federal law, to bolster protection for electronic records
- Creating a process to certify EHR technology, so providers can be assured that the EHR technology they acquire will perform as needed
- Identifying standards for certification of products, tied to “meaningful use” of EHRs
- Identifying the “meaningful use” objectives that providers must demonstrate to qualify for incentive payments.
- Supporting State Medicaid Agencies in the planning and development of their Medicaid EHR Incentive programs with 90/10 matching funds.
Why EHRs?
Electronic health records improve care by enabling functions that paper records cannot deliver:
- EHRs can make a patient’s health information available when and where it is needed – it is not locked away in one office or another.
- EHRs can bring a patient’s total health information together in one place, and always be current – clinicians need not worry about not knowing the drugs or treatments prescribed by another provider, so care is better coordinated.
- EHRs can support better follow-up information for patients – for example, after a clinical visit or hospital stay, instructions and information for the patient can be effortlessly provided; and reminders for other follow-up care can be sent easily or even automatically to the patient.
- EHRs can improve patient and provider convenience – patients can have their prescriptions ordered and ready even before they leave the provider’s office, and insurance claims can be filed immediately from the provider’s office.
- EHRs can link information with patient computers to point to additional resources – patients can be more informed and involved as EHRs are used to help identify additional web resources.
- EHRs don’t just “contain” or transmit information, they also compute with it – for example, a qualified EHR will not merely contain a record of a patient’s medications or allergies, it will also automatically check for problems whenever a new medication is prescribed and alert the clinician to potential conflicts.
- EHRs can improve safety through their capacity to bring all of a patient’s information together and automatically identify potential safety issues — providing “decision support” capability to assist clinicians.
- EHRs can deliver more information in more directions, while reducing “paperwork” time for providers –for example, EHRs can be programmed for easy or automatic delivery of information that needs to be shared with public health agencies or quality measurement, saving clinician time.
- EHRs can improve privacy and security – with proper training and effective policies, electronic records can be more secure than paper.
- EHRs can reduce costs through reduced paperwork, improved safety, reduced duplication of testing, and most of all improved health through the delivery of more effective health care.
Why “meaningful use” requirements?
EHRs do not achieve these benefits merely by transferring information from paper form into digital form. EHRs can only deliver their benefits when the information and the EHR are standardized and “structured” in uniform ways, just as ATMs depend on uniformly structured data. Therefore, the “meaningful use” approach requires identification of standards for EHR systems. These are contained in the ONC Standards and Certification regulation announced on July 13, 2010.
Similarly, EHRs cannot achieve their full potential if providers don’t use the functions that deliver the most benefit – for example, exchanging information, and entering orders through the computer so that the “decision support” functions and other automated processes are activated. Therefore, the “meaningful use” approach requires that providers meet specified objectives in the use of EHRs, in order to qualify for the incentive payments. For example: basic information needs to be entered into the qualified EHR so that it exists in the “structured” format; information exchange needs to begin; security checks need to be routinely made; and medical orders need to be made using Computerized Provider Order Entry (CPOE). These requirements begin at lower levels in the first stage of meaningful use, and are expected to be phased in over five years. Some requirements are “core” needs, but providers are also given some choice in meeting additional criteria from a “menu set.”
Identification of the “meaningful use” goals and standards is the keystone to successful national adoption of EHRs. The announcement of final “meaningful use” regulations on July 13, 2010, marks the launch of the Nation’s push for EHR adoption and use.
Looking ahead
What is the timetable for approving the organizations that will certify EHR systems as qualifying for “meaningful use?”
- ONC anticipates that the first entities will be authorized as ONC-ATCBs before the end of summer.
How soon can we expect certified EHR systems to be available?
- We anticipate that certified EHR systems will be available later in the fall.
How will be the CMS EHR incentive program registration process work?
- Medicare: Hospitals and eligible professionals can register for the program starting in January 2011. Once the programs begin, a link on the Registration web page on http://cms.gov/EHRIncentivePrograms/ will be available. Providers can use this central website to get information about the program and link to the programs’ online registration system.
- Medicaid: The registration process will be the same for the Medicaid Incentive Program as for Medicare. A link on the Registration web page on http://cms.gov/EHrIncentivePrograms/ will be available when the program begins. Eligible Providers under the Medicaid Incentive Program can register at this site whether or not their state has initiated their program yet and CMS will pass their information on the state once the state initiates their program.
How will providers demonstrate that they have achieved the “meaningful use” objectives required by the regulation?
- For 2011, CMS will accept provider attestations for demonstration of all the meaningful use measures, including clinical quality measures. Starting in 2012, CMS will continue attestation for most of the meaningful use objectives but plans to initiate the electronic submission of the clinical quality measures. States will also support attestation initially and then subsequent electronic submission of clinical quality measures for Medicaid providers’ demonstration of meaningful use.
How and when will incentive payments be made?
- CMS expects to initiate Medicare incentive payments nine months after the publication of the final rule. For Medicaid, States are determining their own deadlines for launching their Medicaid EHR Incentive programs but are required to make timely payments, per the CMS final rule. CMS expects that the majority of States will have launched their programs by the summer of 2011.
# # # # #
Standards and Certification Criteria Final Rule:
Fact Sheet
Excerpted from ONC site on July 14, 2010
The Health Information Technology for Economic and Clinical Health (HITECH) Act provides HHS with the authority to establish programs to improve health care quality, safety, and efficiency through the promotion of health information technology (HIT), including electronic health records (EHRs) and private and secure electronic health information exchange.
The HITECH Act directs the Office of the National Coordinator for Health Information Technology (ONC) to support and promote meaningful use of certified EHR technology nationwide through the adoption of standards, implementation specifications, and certification criteria as well as the establishment of certification programs for HIT.
About the Standards and Certification Criteria Final Rule
Two companion regulations were announced today. ONC’s final rule complements a final rule announced by the Centers for Medicare & Medicaid Services (CMS) that defines the minimum requirements that providers must meet through their use of EHRs in order to qualify for payments under the Medicare and Medicaid EHR incentive programs. The ONC rule establishes the required capabilities and related standards and implementation specifications that Certified EHR Technology will need to include to, at a minimum, support the achievement of meaningful use Stage 1 by eligible health care providers under the Medicare and Medicaid EHR Incentive Program regulations.
What Standards and Certification Criteria Mean for Health Care Providers
Both the Medicare and Medicaid EHR incentive programs include a requirement related to certified EHR technology. Under the Medicare EHR incentive program, eligible health care providers may receive incentive payments if they adopt and meaningfully use certified EHR technology (Complete EHR or EHR Modules that have been certified by an Office of the National Coordinator for Health Information Technology-Authorized Testing and Certification Body (ONC-ATCB)). Under the Medicaid EHR incentive program, eligible health care providers may first adopt, implement, or upgrade to certified EHR technology in their first year of the program and receive an incentive payment before having to meaningfully use certified EHR technology. The standards and certification criteria final rule specifies the necessary technological capabilities EHR technology will need to include, for the EHR technology to be certified by an ONC-ATCB. Additionally, it specifies how eligible health care providers will need to use the certified EHR technology to meet applicable meaningful use requirements.
What Standards and Certification Criteria Mean for Developers of EHR Technology
Developers of EHR technology who design their EHR technology in accordance with this final rule and subsequently get their EHR technology tested and certified by an ONC authorized testing and/or certified entity are assured that their EHR technology can be adopted by eligible health care providers who seek to achieve meaningful use Stage 1.For other questions related to the standards and certification criteria, please email onc.request@hhs.gov
Health Care Providers: Key Points
Both the Medicare and Medicaid electronic health record (EHR) incentive programs include a requirement related to certified EHR technology. Under the Medicare EHR incentive program, eligible health care providers must adopt and meaningfully use certified EHR technology (Complete EHR or EHR Modules that have been certified by an Office of the National Coordinator for Health Information Technology-Authorized Testing and Certification Body (ONC-ATCB)). Under the Medicaid EHR incentive program, eligible health care providers may first adopt, implement, or upgrade to certified EHR technology in their first year of the program and receive an incentive payment before having to meaningfully use certified EHR technology. The standards and certification criteria final rule specifies the necessary technological capabilities EHR technology will need to include in order be certified by an ONC-ATCB and subsequently used by eligible health care providers to meet applicable meaningful use requirements.
Developers of EHR Technology: Key Points
Developers of EHR technology who design their EHR technology in accordance with this final rule and subsequently get their EHR technology tested and certified by an ONC-ATCB are assured that their EHR technology can be adopted by eligible health care providers who seek to achieve meaningful use Stage 1.
B. Standards and Certification
B1. What is the standards and certification criteria final rule?
The final rule establishes the required capabilities and related standards and implementation specifications that Certified EHR Technology will need to include to, at a minimum, support the achievement of meaningful use Stage 1 by eligible health care providers under the Medicare and Medicaid EHR Incentive Programs.
B2. What are the major differences between the standards and certification interim final rule and the final rule?
In large part, the final rule is very similar to the interim final rule. However, in response to public comments, the final rule clarifies or revises certain standards and certification criteria. As noted in the final rule, some of the adopted certification criteria were revised to realign with changes to the Medicare and Medicaid EHR Incentive Programs final rule.
B3. What is the difference between a Complete EHR and an EHR Module?
Complete EHR refers to EHR technology that has been developed to meet, at a minimum, all applicable certification criteria adopted by the Secretary. For Complete EHRs designed for an ambulatory setting this means all of the certification criteria adopted at 45 CFR 170.302 and 45 CFR 170.304. For Complete EHRs designed for an inpatient setting this means all of the certification criteria adopted at 45 CFR 170.302 and 45 CFR 170.306. These certification criteria represent the minimum capabilities EHR technology needs to include and have properly implemented in order to achieve certification. They do not preclude Complete EHR developers from including additional capabilities that are not required for the purposes of certification.
EHR Module refers to any service, component, or combination thereof that meets at least one certification criterion adopted by the Secretary. EHR Modules, by definition, must provide a capability that can be tested and certified in accordance with at least one certification criterion adopted by the Secretary. Therefore, if an EHR Module does not provide a capability that can be tested and certified at the present time, it is not HIT that would meet the definition of EHR Module. We stress “at the present time,” because as new certification criteria are adopted by the Secretary, other HIT could be developed and then tested and certified in accordance with the new certification criteria as EHR Modules. An EHR Module could provide a single capability required by one certification criterion or it could provide all capabilities but one, required by the certification criteria for a Complete EHR. In other words, we would call HIT tested and certified to one certification criterion an “EHR Module” and HIT tested and certified to nine certification criteria an “EHR Module,” where ten certification criteria are required for a Complete EHR.
B4. CMS has specified a number of clinical quality measures for meaningful use. What clinical quality measures must EHR technology include in order to be certified?
In order to be certified, a Complete EHR or EHR Module designed for an ambulatory setting must be tested and certified as including at least nine clinical quality measures specified by CMS – all six of the core (three core and three alternate core) clinical quality measures specified, and at least three of the additional measures. Complete EHR and EHR Module developers may include as many clinical quality measures above that requirement as they see fit.A Complete EHR or EHR Module designed for an inpatient setting must include and will be required to be tested and certified to all of the clinical quality measures specified by CMS.
B5. Does EHR technology need to include administrative transactions capabilities?
No, we have removed these capabilities as conditions of certification for EHR technology in support of meaningful use Stage 1, but intend to revisit their inclusion for Stage 2.
C. Certification Process
C1. Where can I find out about the certification process?
For more information on the temporary certification program and the certification process, visit http://healthit.hhs.gov/tempcert.
D. Comments on the Interim Final Rule
D1. Where can I learn about how my comments on the interim final rule on standards and certification criteria, issued in January, were addressed in the final rule?
ONC staff carefully reviewed and considered each of the approximately 400 timely comments received on the standards and certification criteria interim final rule. Section III of the standards and certification criteria final rule discusses how the comments were addressed and incorporated into the final rule.
E. Related Rules
E1. How is this final rule related to the Medicare and Medicaid EHR Incentive Programs final rule?This final rule completes the adoption of an initial set of standards, implementation specifications, and certification criteria, and more closely aligns such standards, implementation specifications, and certification criteria with final meaningful use Stage 1 objectives and measures. Adopted certification criteria establish the required capabilities and specify the related standards and implementation specifications that certified EHR technology will need to include to, at a minimum, support the achievement of meaningful use Stage 1 by eligible professionals, eligible hospitals, and/or critical access hospitals.